Following our six step approach, D-tree and our partners have supported the Malawi Ministry of Health to develop and scale the Digital Village Clinic to strengthen Malawi’s community health system.
Over the past six years, we have been refining our implementation approach as we scale a healthcare transformation project in Malawi from a paper-based solution to a Digital Village Clinic– a digital system with a mobile solution for comprehensive healthcare needs.
The Digital Village Clinic is supported by Health Surveillance Assistants (HSAs) responsible for community health services: community case management, maternal and neonatal health, family planning, nutrition management and more. These HSAs started as Cholera Assistants with the Ministry of Health (MoH) in the 1970s, set up to combat the Cholera pandemic. Having assistants in the community proved successful and their duties increased over time. Their role went from managing a case to an entire clinic, and there are now over 10,000 Health Surveillance Assistants deployed in all districts of Malawi.
The Ministry of Health expectations grew along with the HSA responsibilities. Quality of community services became increasingly important, and HSAs had to report to the Ministry of Health across a range of health areas. It was quickly noted that there was a need for supervisors to ensure that the HSA’s were providing adequate care, reporting accurately and using their resources effectively.
The MoH then established a Senior HSA role, or Supervisor.
Prior to the Digital Village Clinic, there were many healthcare challenges due to the use of multiple paper-based tools: poor quality of care, duplication of HSA work, inefficient data management and lack of care across the continuum. The solution, in moving from paper to digital, has since transformed Malawi health services:
-
Streamlining multiple workflows, guidelines and protocols for community health services into one digital application
-
Integrating with the healthcare system to support health workers, supervisors, ministry officials and project partners with tools and information necessary to provide better services to their communities
-
Supporting content flexibility, depth and breadth after years of growth to a comprehensive portfolio of HSA services. The Digital Village Clinic also supports managerial supervision services and program analysis through on-device reports and dashboards.
But this transformation did not happen overnight. Through our methodical implementation approach, we have worked with the Ministry of Health and other NGOs to drive the solution implementation and ongoing updates. Our approach works to ensure clear understanding of user and project needs as well as support and capacity building through testing, refinement and training. In the figure below and the rest of this post, we demonstrate the process we follow.
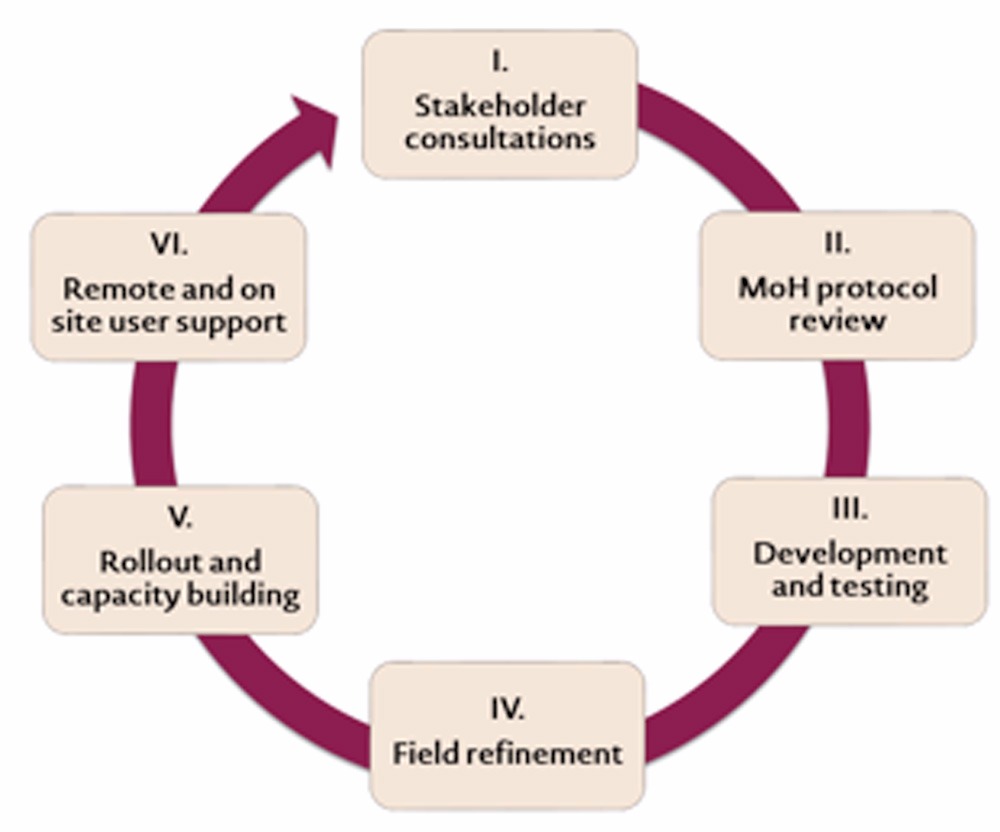
I. Stakeholder consultations
We start every new project or digital solution by consulting with various stakeholders: Ministry of Health, District Health Management Teams, partners and end users. Often we discuss with partner organizations like Save the Children, Jhpiego and Barr Foundation to agree on program scope and targets. We talk about the components of the Digital Health Clinic that they want to adopt, program location, as well as number of users and projected outcomes. For example, during discussions with Save the Children in 2015 (a current parter) about a program in Blantyre, we agreed to implement multiple components for community case management, maternal health and family planning. We discussed their plan to train 145 HSAs and 35 Supervisors, and see better outcomes for maternal health and comprehensive family planning through dashboards and reports. We are flexible in these discussions with partners as we learn about their goals and plan the engagement from solution development to implementation. These discussions are also critical as we meet with end users to understand how the solution will work for their setting.
To fully understand the end user perspective, we shadow HSAs and Supervisors in the field and observe their current processes to recognize how the Digital Village Clinic will change activities. First, we work with individuals at the district level to identify different settings where we can see various workflows. From these sessions, we are able to understand activity gaps as well as user challenges and frustrations, and then incorporate feedback into the solution to address issues
It is incredibly valuable for us to work side by side with end users, partners and the MoH to co-design a solution that best meets the priorities of the government and partner, while considering the impact on the user workflow.
II. Ministry of Health protocol review
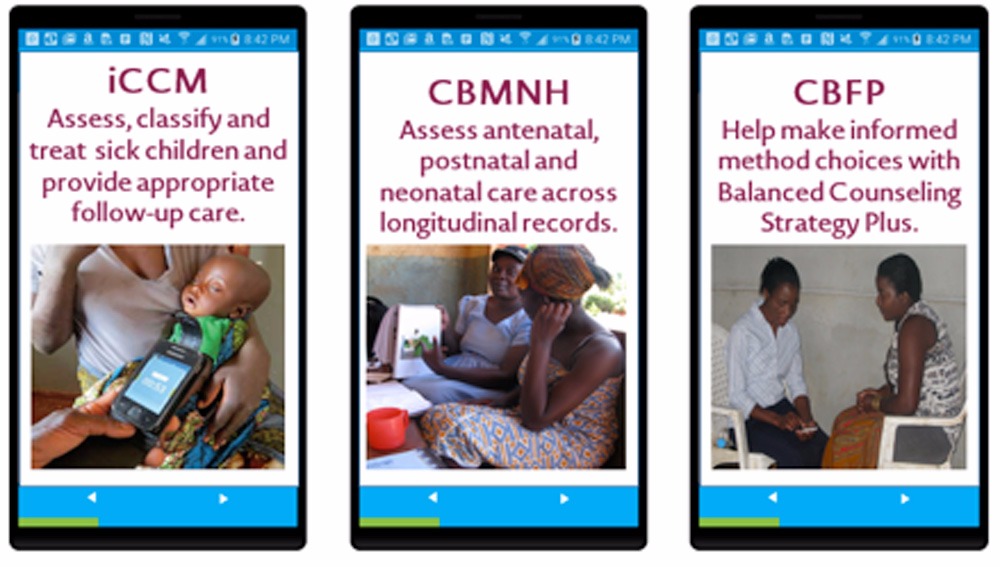
We then review the most current protocol documents and HSA training materials from the Ministry of Health. We incorporate these protocols in the solution to make sure that services and decision support is standard across the program. To date, we have done so for integrated Community Case Management (iCCM), Community Based Maternal and Neonatal Health (CBMNH), and Community Based Family Planning (CBFP).
Often we work with the Ministry of Health to incorporate changes to protocol based on feedback from the field. For example, we adjusted the number of maternal visits required in the Community Based Maternal and Neonatal Health solution from three to two, and made sure the timing of the visits was flexible. Initially, the Ministry protocols required that the HSA must see a mother three times at specific intervals (one time per trimester) before delivery. However, through discussions with users, we found that women were often unable to visit the HSA at specified times because 1.) Their first visit with an HSA was often after the first trimester and 2.) They had trouble seeing the HSA at a specific time during the 3rd trimester.
The first issue was a result of women hiding their pregnancy from others until after the first trimester; they therefore did not visit the HSA until the second trimester. We found that women do this because there is a culture of superstition that they will lose the baby if they reveal a pregnancy to others early. The second issue was because the mother often moved away for delivery, so they needed flexibility about the timeframe of the last visit before delivery.
III. Solution development and testing
After solution development, we continue engagement with the Ministry of Health to support the Digital Village Clinic testing and growth. A team at the Ministry works with us to test and certify the app’s adherence to protocols and provides feedback on the design of the solution and dashboard. The team is made up of Ministry officials that are experts on the program goals. In most cases, these same individuals are engaged throughout the implementation lifecycle, which guarantees continuity and understanding while testing.
IV. Field refinement and feedback
After testing, we engage with end users during a refinement phase where we train a subset of HSAs and supervisors and follow them over a six to twelve week period. We identify and train a small group of users and provide the digital tools to use in their village clinics. We monitor this group closely and gather feedback for protocol, solution and workflow improvement. Before making protocol changes based on this feedback, we consult the Ministry of Health team to validate changes since clinical protocol accuracy is of the utmost importance for quality care. We then develop approved adjustments, and confidently share the app with a larger group of users.
The refinement participants appreciated that we incorporated their suggestions and as a result, felt ownership of the app. This was especially evident two years ago when we underwent a solution migration from one type of software to another. It took users some time to adjust, but eventually they recognized the new software’s ease and flexibility. They were especially engaged after refinement updates; they were happy to claim, “That’s mine” to new parts of the application that we updated based on their feedback. Then, when rolling out to the larger group, refinement participants felt empowered as they shared app updates with others and helped ease the transition for the program.
V. Solution rollout and capacity building

Whenever we roll the solution out to the larger group of HSAs, we make sure to do so thoughtfully and efficiently by applying strategies that we have developed over time. Below are some examples we practice to help engage end users and build MoH and partner capacity.
-
Mobile games to build phone skills- Through training sessions, we discovered that HSAs had trouble tapping and swiping on the screen, a new skill for individuals not familiar with smart phones. To address this, we incorporate phone games into training activities to introduce the swiping/tapping skill. This creates a friendly environment to engage with users and helps them become more comfortable with the phone. By the time they move on to the solution training, users confidently swipe and tap the Digital Village Clinic apps in the same way. Over time we observed that mobile games during training helped improve the tap and swipe skill from about 50 percent to 80 to 90 percent of participants.
-
Flexible training content for the users– We recognize that we need to be flexible with how we conduct training sessions to adjust for various combinations of app components. Some projects only allow individuals to be trained on CCM, but in others, HSAs run three programs and need to be trained on all. Then, within locations where HSAs run three programs, some individuals may only participate in two of the three or one of the three, so we divide the training into groups and adjust the agenda to address these combinations. For example, if all HSAs work on CCM and MNH, but only a subset participate in family planning, we train all groups together for the first three to four days on two components of the app. Then we dismiss everyone except the individuals who use family planning components as well and train that group for the remainder of the week. We also try to keep the size of the group small at 15-20 users, so groups are organized and participants can actively engage.
-
Partner Training of Trainers for capacity building– Training of Trainers is one strategy we use to build capacity of the Ministry and our partners. We train a subset of MoH colleagues who then train others on the solution. Over time this has become a mandatory activity for many district level coordinators, which is critical because in the past, they did not fully engage or understand the solution well. Through Training of Trainers, coordinators are accountable for the solution performance. They are encouraged to train and support HSA’s not only in the programs that they lead, but in all aspects of the Digital Village Clinic. We build their capacity to ensure sustainability in that they take ownership of the solution and are able to continue using it and supporting users with minimal to no support.
VI. Remote and on site user support

As soon as the HSAs and supervisors begin to use the solution, we work with them to plan follow-up activities, including village clinic visits, to observe and support HSAs in their work. We, along with supervisors, provide real-time feedback during the visits, and identify areas that need improvement and follow up. At times where there is no onsite supervision, we help HSAs follow an established chain of reporting for support, so their issues are addressed in a timely matter. HSAs express any challenges to their supervisor, who resolves them or reports them to a coordinator. Coordinators then direct any escalations to us to analyze and provide a final solution.
This issue support structure builds the capacity of coordinators and supervisors as they work to resolve issues and familiarize themselves with the Digital Village Clinic. We observe that over time, we receive fewer issues as coordinators and supervisors are able to resolve items without escalating to us. For instance, initially after training we usually see about 30 issues reported to us in a day. A few months later, that number decreases to about 10 as coordinators and supervisors build capacity to address issues.
In addition to issue resolution, we provide ongoing support and follow up with staff and users to understand technical and workflow challenges, and help to plan for re-design for the next phase of work.
The implementation lifecycle will be an important tool for the Ministry of Health as they continue digital health efforts. According to the National Community Health Strategy for 2017-2022, the Malawi Ministry of Health aims to have 50% of community health teams in Malawi using mHealth for service delivery, data collection and supervision by 2022. By applying the six implementation steps, and continuing to keep close partnerships and community ties, the Malawi Digital Village Clinic will be able to successfully continue scaling for comprehensive program improvement.
