This post is part of our ongoing Digital Spark series. Be sure to also check out the series introduction as well as the other posts in the series: setting digital health apart, embracing collaboration, data protection and privacy, and lessons from COVID-19.
As we celebrate the progress that has been achieved globally, we also recognize that the work is not yet done. In looking back over the past twenty years, we recognize that although large populations have lifted themselves out of poverty and achieved strong health systems, other populations have not advanced at the same rate. It has become evident that global gains in health have not been equitably realized, and large health gaps remain—particularly for low-income and marginalized populations.
As we celebrate the progress that has been achieved globally, we also recognize that the work is not yet done.
Despite global advances, many countries have witnessed slow progress in health improvements and still experience high rates of child mortality and an unmet need for family planning with stagnant reductions in communicable diseases and preventable maternal deaths. At the same time, the prevalence of non-communicable diseases such as diabetes, heart disease, and cancer, continues to rise and we are witnessing the real risk and consequences of epidemics as populations are more mobile than ever before. Despite progress, it is evident that traditional approaches applied over the past decades to address global health problems in these settings are not working fast enough.
The global shift toward health systems strengthening
With heightened urgency for reducing health disparities and recognized shortcomings of past approaches, world leaders are looking to adopt a more holistic global health approach—namely, a health systems strengthening approach. Global health leaders recognize that while there is evidence that health interventions can prevent many diseases experienced in underserved settings, fundamental problems with broader health systems inhibit the interventions from being delivered efficiently and effectively.
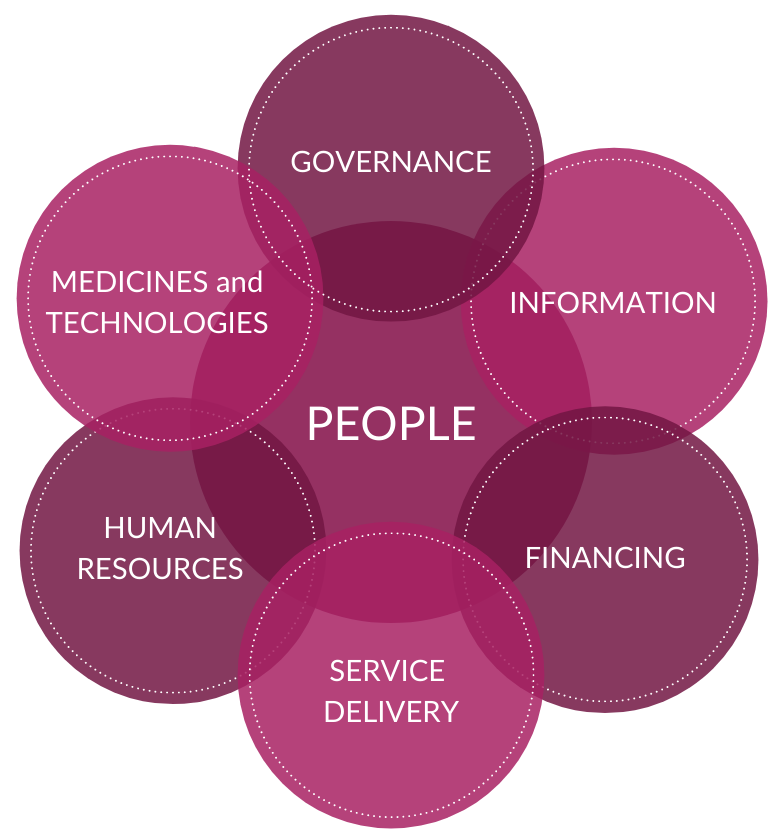
According to the WHO, health systems strengthening is defined as “improving [the] six health system building blocks and managing their interactions in ways that achieve more equitable and sustained improvements across health and health outcomes.” Furthermore, a systems thinking approach to health “views problems as part of a wider, dynamic system. Systems thinking involves much more than a reaction to present outcomes or events. It demands a deeper understanding of the linkages, relationships, interactions and behaviours among the elements that characterize the entire system.”
The WHO has asserted the necessity of employing a health systems strengthening approach to achieve universal health coverage by 2030 and called for health system strengthening efforts to be scaled up immediately.
Digital technology as a catalyst
While global leaders are calling on a health systems approach to achieve Sustainable Development Goal targets, another lever being touted as the key to acceleration in health gains is digital technology. At the 2016 World Economic Forum, the growth of digital technology was declared as the “Fourth Industrial Revolution,” and the WHO has highlighted digital technology as essential for achieving the Sustainable Development Goals, including universal health coverage.
In reference to digital technology, the WHO declared that “such technologies are no longer a luxury; they are a necessity.” They affirm that digital technology introduces opportunities to address health system challenges and offers the potential to improve the coverage and quality of health care services. A 2018 WHO Member States Resolution urged ministries of health to prioritize considering expanded applications and use of digital technologies, particularly while designing health system reforms.
Harnessing the joint potential of health systems strengthening and digital technology
In order to achieve the ambitious and urgent Sustainable Development Goal targets—including universal health coverage—a holistic yet innovative approach is required. Global health experts recommend a health systems strengthening approach and urge countries to explore how the application of digital technology may expedite the change process and more efficiently improve the accessibility and quality of health services.
The question is how. How can digital technologies be deployed in a way that fosters systems strengthening, rather than fragmentation? To date, only a few examples exist. Historically the excitement to employ digital technology has led to a proliferation of short-term digital tools without much attention to their impact on health systems or how health system limitations might impede the effectiveness or longevity of the intervention. Instead, a better approach to digital health is to review the health systems needs and context before designing a digital intervention.

A health systems approach in practice
When employing a holistic health systems strengthening approach to digital health, the following best practices can act as starting points for conceptualizing or strengthening digital health interventions:
-
Explore the details around the health problem—why does it exist, what’s been done to resolve it to date, and what are the key challenges inhibiting improvement?
-
Seek to understand the context of the specific locality—including culture, infrastructure, and economic constraints—to gain additional insight into the challenges and as key considerations in ideating potential solutions. Speak with multiple stakeholders, including beneficiaries, health providers, policymakers, and community leaders in order to attain diverse perspectives and work hand-in-hand with local experts, including governments and partner organizations throughout the process in order to understand the challenges and context more fully and to foster a locally-derived and relevant solution.
-
Recognize that each problem uncovered is multi-faceted and part of a larger system. Seek to understand the linkages and interactions among challenges, in order to select where it may be most effective to intervene and consider how to foster an appropriate supportive environment to sustain and promote the intervention.
As D-tree staff with expertise in digital health, we bring a unique contribution to these exploratory efforts. As a balanced team of public health and technology experts, we start each endeavor by focusing on the health problem and the context around the challenge to be resolved. Once we understand the problem, contextualize its relation to the larger health system, and begin to work with governments and partners to devise an intervention to alleviate the problem, we propose options for how technology could play a role in alleviating the constraints identified. As a D-tree team, we consider opportunities to employ digital technology to expedite or amplify the effectiveness of an intervention and share these considerations with our partners. We present innovative technology options—including pros and cons of various software and hardware—and, given local needs and realities on the ground, we lead a conversation around feasibility, systems integration, impact, maintenance, and sustainability. In doing so, we help governments and health system actors make informed and strategic decisions around employing digital technology to bolster health interventions.
The effectiveness of this health systems strengthening approach can be illuminated by three distinct examples of digital strategies within the global health sphere:
i. Emergency transport
In rural Tanzania, access to health facilities for mothers and babies during the delivery and postpartum period is a major challenge, contributing to high rates of maternal and newborn mortality. D-tree is working with the Touch Foundation and Pathfinder International to address this issue through an innovative emergency transport system that has been integrated into the government health system to ensure that no mothers and babies die due to lack of transport during life threatening emergencies. A 24-hour toll free number has been set up, linking callers with a dispatcher who is supported by a mobile app. The mobile app helps to triage the condition, determine if an emergency exists and the nearest health facility equipped to manage that condition, and identify government ambulances or local taxi drivers who can quickly collect the mother and transport her to the relevant health facility. Drivers are then paid via mobile money, and the dispatcher records information in the mobile app about outcomes of the case to improve the system and support government-led data for decision making. This system has provided life-saving transport to more than 10,000 mothers and babies and has demonstrated a 27% reduction in maternal mortality. It is currently being scaled to cover the entire Shinyanga Region in northwest Tanzania, with the local government increasingly taking on operational oversight and payment for transportation, and plans are in place for broader scale-up.

ii. Health hotline
Malawi has one of the highest maternal, child, and infant mortality rates in the world, and yet people in remote rural Malawian communities are often too far from health centers to have reliable access to the health care that they need. In 2011, however, VillageReach turned this model on its head by finding a way to provide essential health services even in remote and rural communities. Together with the Malawi Ministry of Health, VillageReach developed the Chipatala cha pa Foni (CCPF) program. CCPF acts as a toll-free general health hotline to link people in rural areas with trained health workers who can provide referrals and education on topics such as nutrition, health promotion, illness prevention, health seeking behaviors, and sexual reproductive health. Pregnant women can also sign up for a mobile messaging service for tips and reminders, thereby further increasing this vulnerable group’s contact with the health system. By 2018, users of the CCPF program were more likely to utilize antenatal care, receive HIV testing, use contraceptives, and have greater nutritional knowledge. The CCPF program has now scaled to all 28 districts of Malawi, and VillageReach is in the process of transferring all operations to the Ministry of Health so that the government can fully own and operate this national health hotline system
iii. Financial empowerment
At the beginning of this year, approximately 700 million people across the globe were living in extreme poverty. As COVID-19 seeps into communities across the world, this number could jump to more than 770 million. BRAC is attempting to significantly combat extreme poverty through the scale-up of their Graduation project. This project works with governments to enact systems-level change by focusing on assistance across four key pillars: meeting basic needs, income generation, financial support and savings, and social empowerment. Working interdependently, interventions address these pillars holistically and work with individuals at the household level to “graduate” out of extreme poverty. Due to the initial success of the program, BRAC was selected by The Audacious Project to scale up their model to work with 4.6 million households—over 21 million people— over the next 6 years.
Technology, when coupled with health systems strengthening efforts, can play a powerful role in expediting change and maximizing health impact.
The organizations behind each of these seemingly disconnected examples take the same approach: they holistically examine the challenge in the unique context where it occurs, they recognize and learn from what has and hasn’t been successful in the past, and they seek to work with and connect the various parts of the health or government system to achieve significant impact. These projects, and those like them, have affirmed our belief that technology, when coupled with health systems strengthening efforts, can play a powerful role in expediting change and maximizing health impact. Though there are countless digital strategies—digital referral systems, health hotlines, digitally-enabled transportation services, and financial empowerment tools are just a few—there is no longer any doubt, within the global health community, that these strategies must be responsibly and cooperatively integrated into health systems strengthening initiatives if we are to meet the Sustainable Development Goals and work toward achieving universal health care.
Photography by Mark Leong/Professional WHO Photographer and Kevin Ferguson
References
The Audacious Project. (2020). Retrieved July 08, 2020, from https://audaciousproject.org/
Blauvelt, C., West, M., Maxim, L., Kasiya, A., Dambula, I., Kachila, U., . . . Armstrong, C. E. (2018). Scaling up a health and nutrition hotline in Malawi: The benefits of multisectoral collaboration. Bmj. doi:10.1136/bmj.k4590
A Digital (r)Evolution: Introducing The Lancet Digital Health. The Lancet Digital Health, vol. 1, May 2019, www.thelancet.com/pdfs/journals/landig/PIIS2589-7500(19)30010-X.pdf.
Don de Savigny and Taghreed Adam (Eds). Systems thinking for health systems strengthening. Alliance for Health Policy and Systems Research. World Health Organization; 2009
Everybody’s business: strengthening health systems to improve health outcomes: WHO’s framework for action. World Health Organization; 2007
The GoalKeepers Report. Bill and Melinda Gates Foundation; 2018. https://www.gatesfoundation.org/goalkeepers/report/2018-report/
GRADUATING 21 MILLION MORE PEOPLE OUT OF EXTREME POVERTY. (2020). Retrieved July 08, 2020, from http://bracultrapoorgraduation.org/audacious/
Healthy systems for universal health coverage – a joint vision for healthy lives. Geneva: World Health.
Organization and International Bank for Reconstruction and Development / The World Bank; 2017.
Seventy First World Health Assembly Agenda Item 12.4 Digital Health. 26 May 2018.
Schmets G, Rajan D, Kadandale S, editors. Strategizing national health in the 21st century: a handbook. Geneva: World Health Organization; 2016. Handbook.
The Stories Behind the Data. Bill and Melinda Gates Foundation; 2018. https://datareport.goalkeepers.org/
Sustainable Development Goal 3. United Nations; 2020. https://sustainabledevelopment.un.org/sdg3
WHO guideline: recommendations on digital interventions for health system strengthening. Geneva: World Health Organization; 2019. Licence: CC BY-NC-SA 3.0 IGO.
World Report on Health Policy and System Research. World Health Organization; 2017.
Xu K, Soucat A & Kutzin J et al. Public Spending on Health: A Closer Look at Global Trends. Geneva: World Health Organization; 2018.

