Article Preview
-
Jamii ni Afya is a nationwide community health volunteer program in Zanzibar led by the Ministry of Health and local authority (PORALGSD), supported by D-tree International, and funded by key partners such as Fondation Botnar and HDIF. The MOH launched Jamii ni Afya as part of its revised National Community Health Strategy on February 5.
-
Born from the successes of the Safer Deliveries program (2013-2019), the Jamii ni Afya program utilizes technology as the foundation of the care delivery and monitoring system to bring quality care into communities and homes.
-
Jamii ni Afya has been rolled out in two districts so far as part of a soft launch to gather learning before scaling further. In these areas, 300 CHVs and 36 supervisors are already serving over 150,000 people. The program is set to achieve nationwide coverage in all eleven districts by 2021.
-
Community health is a critical link between families and the health system, and is essential to the improvement of household health care decision-making, care-seeking practices, and improving behaviors to promote well-being. In the future, the Jamii ni Afya model could be applied to other areas of health and health systems strengthening globally, even beyond the community level.

This month, the Revolutionary Government of Zanzibar’s Ministry of Health (MOH), together with the local government authority [1], launched the Jamii ni Afya (translated as, “Communities are Health”) program at the Zanzibar Joint Annual Health Sector Review meeting as part of the revised National Community Health Strategy. Jamii ni Afya is a nationwide community health volunteer program that utilizes technology as the foundation of the care delivery and monitoring system. Spearheaded by the government, supported by D-tree International, and funded by key partners such as Fondation Botnar and the Human Development Innovation Fund (HDIF, a UKAID innovation program in Tanzania), the Jamii ni Afya program will be introduced to all eleven districts of Zanzibar and equip a total of 2,200 Community Health Volunteers (CHVs) to provide essential health promotion, counseling, and referral services for all of Zanzibar’s 1.5 million residents. This program introduces a transformative model to the global healthcare stage, as it is the first digital community health program to promise nationwide coverage for all its citizens—a key milestone on the path to Universal Health Coverage.
Program Background
This impressive feat is the result of nearly a decade of work and collaboration. In 2010, the Zanzibar government began a partnership with D-tree International through a small pilot program called “Safer Deliveries.” The program provided existing CHVs with a digital tool that addressed the complex barriers that too often kept pregnant women in rural areas from delivering safely at health facilities— barriers such as lack of transportation, insufficient financial preparations, and difficulties in obtaining customary permissions from male partners.

Even in its infancy, the Safer Deliveries program demonstrated the potential of digital technology to radically transform the quality of a health system and soon scaled to 10 of Zanzibar’s 11 districts, serving over 80,000 pregnant women from 2013-2019. By the end of the Safer Deliveries program in September 2019, healthcare facility delivery rates had improved, postpartum care-seeking behavior had increased, CHVs were able to identify and refer at-risk pregnant women and newborns, and referral completion rates increased threefold compared to non-digital CHV programs [2].
Given these promising initial results, the government chose to formally adopt and expand the digital community health system into its revised National Community Health Strategy (2019-2025). The Community Health Strategy serves as a formal MOH strategy document outlining how CHVs fit within the larger Zanzibar health system and specifying their roles, responsibilities, training, and required qualifications.
Significantly, this revised Community Health Strategy specifies that CHVs will be supported with a digital health platform, as the MOH recognized the benefits of technology in the pursuit of its vision for a healthy population. A digital tool allows for scheduling and management of the considerable workloads of CHVs serving hundreds of clients in a wide range of services—including not only maternal and newborn health services, but also key elements of child health such as nutrition, immunizations, and early childhood development. An agile digital tool also leaves open the possibility of integrating additional health areas in the future, such as non-communicable diseases, family planning, adolescent health, or mental health. Finally, a digital system allows the MOH to transform global evidence and national policy into conversations and care in the home; to track clients and families’ care and outcomes over time; to prioritize those with greatest need; and to have real-time monitoring by supervisors and managers.
And so, faced with the daunting task of digitizing a community health volunteer program on a national scale, we set out to build technology would meet the needs of a comprehensive system serving as the backbone of Zanzibar healthcare at the community level. We knew, however, that building technology to improve the efficiency, quality, and accountability of health systems does not mean just building a singular app for CHV visits. CHVs are one important component of the healthcare machine, but they are just one component—and designing for a system means designing for the whole system
Designing the Current System
The launch of Jamii ni Afya comes after a year of detailed planning and design of the system the government envisioned: a system responsive to the needs of the Zanzibari population and local context. We followed a Human-Centered Design model, meaning that from the outset, stakeholders—including beneficiaries, CHVs, and various levels of government staff—were actively involved in designing and developing program structure, content, and digital tools.
In late 2018, we began meeting with MOH stakeholders, CHVs, and development partners to design the household registration and visit workflows, application information architecture, and application prototypes. During these workshops, we also solidified the scope of the service delivery package to include early childhood development, nutrition, immunizations, and Reproductive Maternal Neonatal and Child Health services.

Designing these elements in parallel, we followed a Minimum Viable Product approach; that is, we started with a simple, bare-bones skeleton of the app with the functionalities necessary to run a basic version of the program, then added more as we tested and received feedback. This approach has allowed us not only to make meaningful community health services available early, but also to gather user feedback for the continuous improvement and expansion of the digital tools and system.
In addition to their involvement in app design, the MOH and District Health Management Teams have been critical to program planning, strategy, implementation, and continued monitoring and management. By engaging in co-creation and co-implementation of Jamii ni Afya, the government has gained firsthand experience in managing the program and technology from the start. This experience will lend itself to enhanced government capacity for continued ownership over the program and the sustainability of Jamii ni Afya as part of the government health system.
Jamii ni Afya is Born
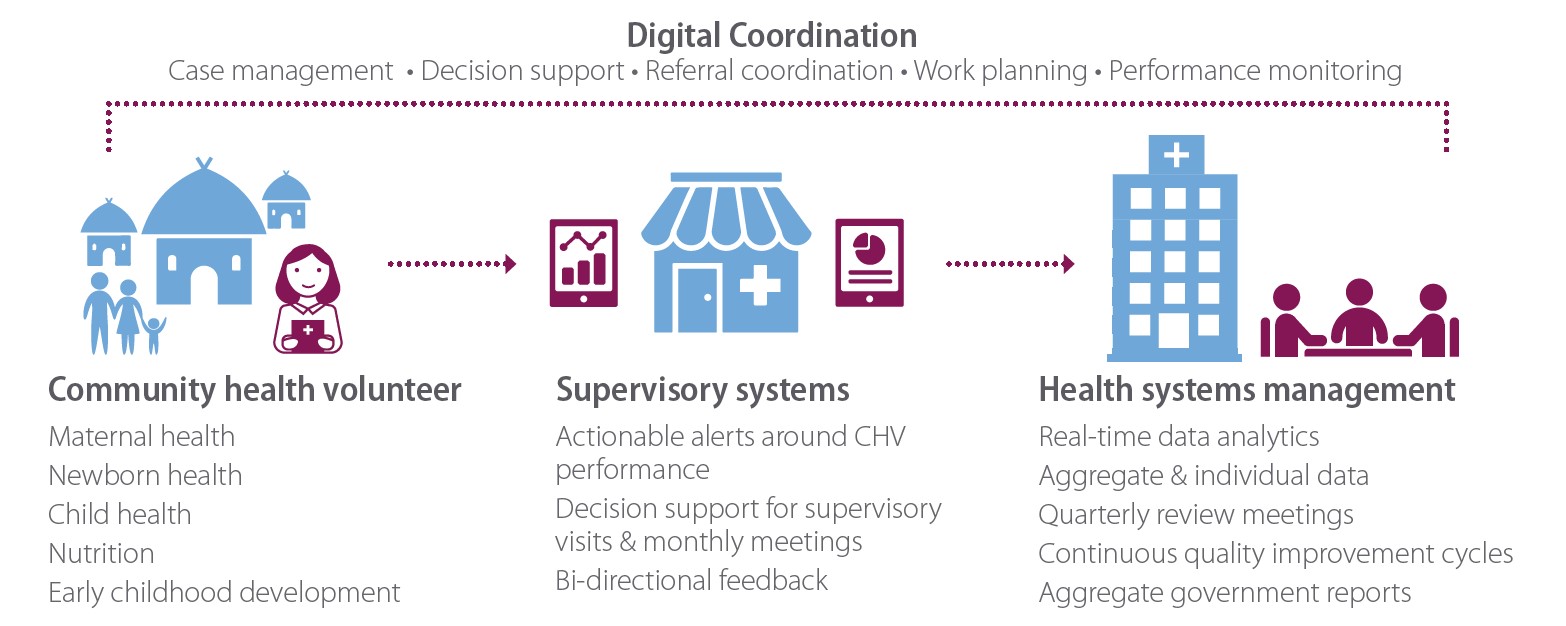
The product of this extensive, collaborative design process is Jamii ni Afya: a national community health program featuring a digital system that supports not only CHVs, but also their health facility-based supervisors as well as the district- and national-level managers. The Jamii ni Afya CHV mobile app was built using the Community Health Toolkit platform—an open source global good with a large network of users and contributors. The tools within the digital system ensure that:
-
CHVs are providing high-quality, tailored services in nutrition, early child development, and Reproductive Maternal Neonatal and Child Health;
-
CHVs can track and respond to the needs of the families they serve over time;
-
CHV performance is measured consistently, and CHVs are compensated appropriately and on time;
-
Supervisors based at health facilities can monitor CHV work remotely in real-time and respond to CHV needs;
-
Government health managers can identify priority health areas based on community-level data and incorporate this into planning, budgeting, and supportive supervision activities; and
-
Communities have a voice in the health system and can provide feedback on the quality of services they receive at health facilities
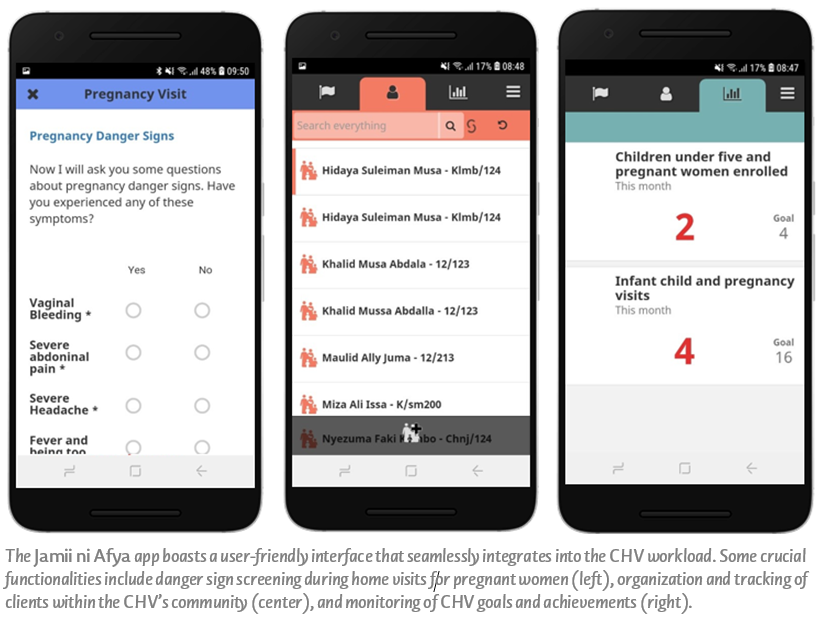
The information collected from these tools is designed to be accessible and reliable for the people who need it most. Supervisors and CHVs will have at their hands a wealth of data about the health services offered, trends in behaviors, gaps and needs, and feedback from communities. District Health Teams will be able to use this data to answer questions and inform routine performance reviews and supervision plans. National managers will be able to monitor CHV workload and trends in service delivery, helping to inform decision-making that can improve community health service delivery, and, ultimately, health outcomes. “Our health facility supervisor is able to see what we do in the community,” said one CHV about the benefits of the Jamii ni Afya app. “The app automatically updates our information, and the supervisor usually calls and asks if she doesn’t see our work. This arrangement has helped me cross-check my data sync and performance.”

The Latest
In the wake of the official launch of the Community Health Strategy earlier this month, the MOH, local government authorities, and D-tree are now working to promptly and efficiently roll out the Jamii ni Afya program throughout Zanzibar. Since the initial soft launch in July of 2019, designed to gather feedback before scaling further, the system has already been rolled out in two districts. In these areas, 300 CHVs and 36 supervisors are already serving over 150,000 people.
“We see ourselves as professionals. Being able to use the Jamii ni Afya app improved my work. I [used to] work for an hour in a household [registering] three people, but with this app, I can register 15 people in 20 minutes. I appreciate the digital platform.” –Community Health Volunteer
As Jamii ni Afya enters its third district, we will continue to smooth out the wrinkles of this expanding fabric that will, by early 2021, blanket all eleven districts of Zanzibar. One area of interest as we refine the program is the incorporation of predictive analytics. Using the data from the Safer Deliveries program, we have worked closely with N/LAB at the University of Nottingham to first predict the drivers for perinatal mortality; from there, we have made significant progress on system modeling for future predictions and are continuing to refine these techniques. The next step will be to work with the government to consider whether we can apply the learnings to improving child health outcomes in Zanzibar.

Though the current Jamii ni Afya system is significantly more expansive than its Safer Deliveries predecessor in terms of services provided, there are still more services that to the government is interested in integrating into the system in the future, including adolescent health, mental health, family planning, non-communicable diseases, and further identification and prioritization of households with the greatest health concerns.
The long-term vision for Jamii ni Afya is for the government of Zanzibar to have the capacity and resources to lead and manage the national community health program as a part of its health system. We expect community health to become the very backbone of Zanzibar’s health system, as it lends itself to improving health care decision-making, care-seeking practices, and behaviors at the community level; which, in turn, will help the government achieve its national health targets.
The approach that our team has taken when designing, implementing, and scaling Jamii ni Afya is the same approach that D-tree applies globally. We build or strengthen systems that meet the needs of users at all levels; that add value to their work; that follow an understanding of local needs, context, and opportunities; and that are embedded within existing health system roles and processes.
As a team, we are honored to partner with the Government of Zanzibar in designing and implementing a national program that is intended to be part of its on-going health system. Jamii ni Afya represents an exciting collaborative effort that could, in the future, be applied to other areas of health and health systems strengthening globally, even beyond the community level.
-
President’s Office of Regional Administration, Local Government, and Special Departments (PORALGSD)
-
Peterson, S., et al. Coping with paediatric referral—Ugandan parents’ experience. Lancet. 2004 Jun 12; 363(9425):1955-6.

